Abstract
Sickle cell disease (SCD) is the most common hemoglobinopathy affecting 100,000 people in the United States. Although without a national registry, the precise number remains an estimate and the mortality data remains unknown. The life expectancy of SCD has extended into adulthood with the advent of prophylactic penicillin use, antipneumococcal vaccines, newborn screenings, and use of hydroxyurea (HU). However as SCD patients age, comorbidities arise reducing the life expectancy.
There is an evolving landscape regarding SCD therapies, with 3 FDA approved drugs since 2017 (L-glutamine, voxelotor, crizanlizumab) joining HU which was approved in 1998. It is paramount to understand the factors that lead to early mortality in SCD so that future therapies and cures can be accessible and benefit all SCD patients. We embarked a review of the mortality data in a healthcare system serving a significant number of SCD patients in Atlanta, GA.
Methods:
We conducted a retrospective chart review of the Georgia Comprehensive Sickle Cell Center at Grady Health system's electronic medical record for deceased sickle cell patients from 2013 to 2020. Patients were then grouped into 3 groups, those whom followed up at the Sickle Cell Center (defined as outpatient visit within 6 months prior to death-RF), those whom did not (defined as outpatient visit > 6 months-NF), and those with unknown status.
Results:
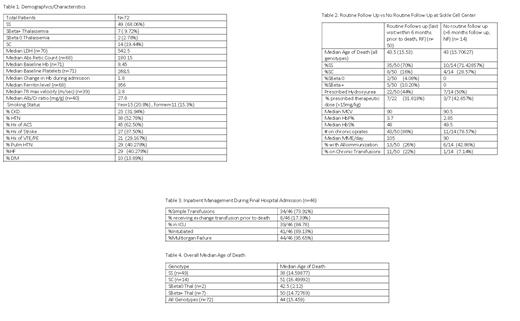
Overall, 72 patients were analyzed, with the following genotype distribution: SS n=49, SC n=14, Sbeta null thalassemia (Sβ0 thal) n=2, SBeta plus thalassemia (Sβ+ thal) n=7. Overall, the most common SCD complication was acute chest syndrome (ACS) (62.5%). The majority had hypertension (HTN) (52.8%), followed by reported heart failure (40.3%) and pulmonary HTN (pHTN) (40.3%), stroke (37.5%), and chronic kidney disease (CKD) (31.9%). 35% were current and/or former smokers. Median TR max velocity was 2.8 m/sec, median albumin/Cr ratio was 27.8 mg/g, and other characteristics are in Table 1.
The median age of death was 44 (STD= 15.5) overall and by genotype it was: SS at age 38 (STD=14.6); Sβ0 thal at age 42.5 ( STD=2.12); Sβ+ thal at age 50 ( STD=14.7); SC at age 51 (STD=16.5). 46 patients had data of their final hospitalization available. 73.9% (n=34) received at least 1 simple transfusion with a only 17.4% (n=8) receiving an exchange transfusion. The majority were critically ill, with 84.8% in the ICU and 95.7% with multiorgan failure.
50 patients had routine follow up (RF) while 14 patients did not (NF), and 8 patients with unknown outpatient visit status. The median age of death for RF and NF were the same 43.5 (STD=15.53) & 43 (STD=15.71) years, respectively. The genotype distribution, and other characteristics are listed in Table 2. About 44% (n=22) of the RF group were prescribed HU, with 31.8% (n=7) were prescribed a dose > 15mg/kg/dose. This was not a significant difference from the NF group, where 50% (n=7) were prescribed HU, with 42.9% at > 15mg/kg/dose. The median MCV, percentage of HbF were similar. Significant majority in RF and NF groups were prescribed chronic opiates (86% and 78.6%, respectively) with 105 and 95 median MME per day. 42.9% of patients in the NF group had alloimmunization compared to 26% in the RF group.
Discussion:
Most of the patients had at least 1 severe complications from SCD, and most had other comorbidities (Table 1). This is commensurate with SCD literature showing that the manifestations of chronic end-organ damage increase as patients age which increases the likelihood of early mortality. In our analysis, the median age of death was similar for those in the RF and NF groups across genotypes.
HU is a disease-modifying therapy that impacts survival and reduces complications and was FDA approved in 1998, however less than 50% of patients had a prescription. Median HbF and MCV were similar between the 2 groups, suggesting HU adherence was not a factor. This raises concern about accessibility of HU for patients which was not within the scope of this review. Improvement of access and education for patients and clinicians of these therapies is needed to see reduction in mortality. As more of the adult population starts to include those with access to HU since early childhood, future studies can examine what impact that will have on HU adherence, and life expectancy. With the advent of new therapies, it is imperative to study these agents on the patients with SCD complications to evaluate their efficacy in reducing mortality.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal